#HarshithaSimhadri #Cardiovascular #Epidemiology #Genetics #Heartdiseases #CircadianRythms #GeneAlterations #Pathophysiology #AlternativeSplicing
Abstract
The heart is one of the most important organs only second to the brain. That is why we should protect it from cardiovascular diseases (CVDs). The four main types of CVDs are coronary heart disease, stroke, peripheral arterial disease, and aortic disease. Through the ages, there have been a lot of revolutions in medications and surgeries. Now in society, there is a wide range of surgical treatments or medicines to help with conquering heart disease. Specialized doctors called cardiologists to help in taking care of the heart and the blood vessels that surround it. Doctors are hopeful that there also will be more advanced and efficient future medications that stop CVDs from the gene level getting rid of errors in the gene code. Though the best way to help your heart now is by making sure you have the right amount of nutrition, sleep 8-10 hours each day, do not smoke and regularly exercise. Heart exercises go hand in hand with breathing exercises and are one of the best ways to protect and nourish your heart. Double checking the health of your heart is also important from time to time, using an electrocardiogram, which is a test that processes the heart’s electrical rhythm and activity is crucial.
Introduction
Annually, around the world, millions of people are affected by cardiovascular disease. Cardiovascular disease is a type of disease that affects the heart or blood vessels. The risk of certain cardiovascular diseases may be increased by smoking, high blood pressure, high cholesterol, unhealthy diet, lack of exercise, and obesity-which are all serious health issues faced by modern society. Of the numerous varieties of the disease, the four most major branches are heart attack, heart failure, heart muscle disease (cardiomyopathy), and heart valve disease. An estimated 16.3 million Americans aged 20 and older have CHD, with a prevalence of 7 percent. The prevalence for men is 8.3 percent and for women is 6.1 percent. One person dies every 36 seconds in the United States from cardiovascular disease. About 659,000 people in the United States die from heart disease each year—that’s 1 in every 4 deaths. Heart disease cost the United States about $363 billion annually from 2016 to 2017. Cardiovascular disease is transmitted through genetic and hereditary factors (race, antecedents, dyslipidemia, high blood pressure, diabetes). Evidence supports that ecological features such as the diurnal cycles of light and day, sunlight exposure, seasons, and geographic characteristics of the natural environment such as altitude, latitude, and green spaces are important determinants of cardiovascular health and CVD risk. In highly developed societies, the influence of the natural environment is moderated by the physical characteristics of the social environments, such as the built environment and pollution, as well as by socioeconomic status and social networks. These attributes of the social environment shape lifestyle choices that significantly modify CVD risk. Cardiovascular disease specifically affects the older generations mainly because older people have aged faster, causing increased stiffness of the large arteries, called arteriosclerosis or hardening of the arteries. This causes high blood pressure, or hypertension, which becomes more common as we age, leading to more probability of cardiovascular diseases.
History of CVD- From Egypt to the 21st Century
Cardiovascular disease, having been dated back to the time frame of ancient Egyptian pharaohs, has been circling since the past and is still a recurring problem as of now in the present society. According to the American college of cardiology, the earliest documented case of CVD (cardiovascular disease) or atherosclerosis was between 1580 and 1550 BC and was found in an ancient Egyptian princess. The Egyptian princess died of a heart attack caused by the build-up of plaque in her arteries. For the next 3500 years, there was little anyone could do to stop CVD. It was only until the U.S.A 34th president’s death from a heart attack did people start to care and realize the truth about CVD. In the early 1960s, Bethany Hospital in Kansas implemented the first coronary care unit, which greatly decreased mortality rates of CVD and soon spread to be included in hospitals all over the U.S. Coronary care units, including the first portable defibrillator, which would shock electricity into people’s hearts to save them from cardiac arrest. Then in the early 1970s, surgeons were able to perform coronary revascularization with angioplasty and bypass surgery which was a major game changer. Other minor advances like Cardiac Ablation were discovered until, in 2012, they discovered new ways to help patients with CVD like TAVR, LVAD, and WATCHMAN to eliminate the unnecessary risks of open-heart surgery. Recently in modern society, cardiovascular healthcare treatments and equipment have been advancing and improving to benefit the welfare of humanity.

Figure 1: This line graph shows the decline of major heart diseases after the development of treatment for CVD. As seen, the progression of the disease elapsed over different time periods in history and is mainly positive and highly elevated in rates of deaths before major advancements have been made.
Types of Cardiovascular Disease and Effects
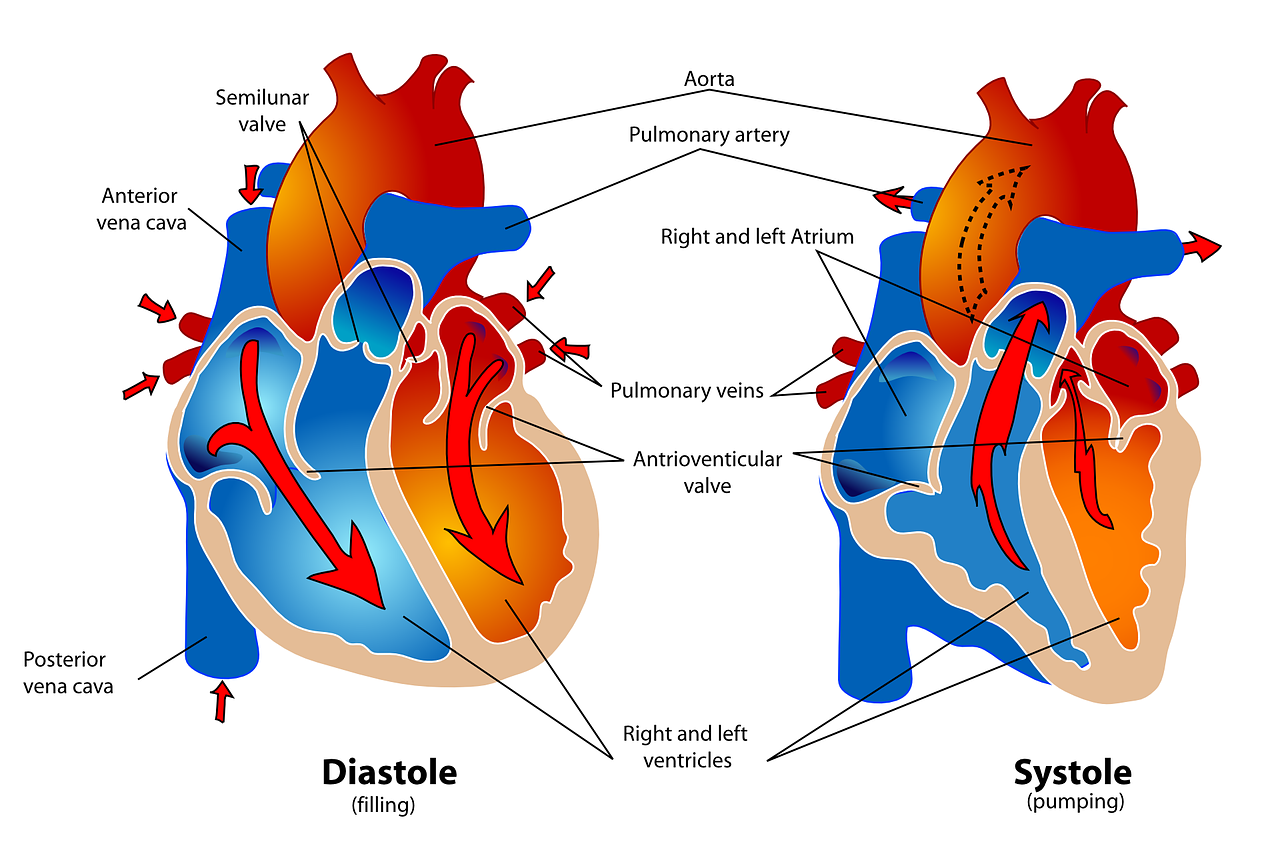
CVD is a large topic that can be divided into four subtopics of major disease categories. The four types are coronary heart disease, stroke, peripheral arterial disease, and aortic disease. Coronary heart disease is a disease that occurs when the muscle around and in the heart’s blood supply is blocked or interrupted by a build-up of fatty substances (atheroma) in the coronary arteries. The coronary arteries supply your heart with blood. If your coronary arteries become narrow due to a build-up of atheroma, the blood supply of the muscles around and in your heart will be restricted. This can cause angina (chest pains). If a coronary artery becomes completely blocked, it can cause a heart attack. The next category is stroke. A stroke is a serious medical condition that occurs when the blood supply to the brain is disturbed. Your brain needs a constant supply of oxygen and nutrients to function properly provided by blood. If your blood flow is restricted or stopped, brain cells will begin to die. This can lead to brain damage and possibly death. Therefore, a stroke is a medical emergency and must be treated fast. Symptoms of stroke include weird facial gestures, including the face may have drooped on one side, the person may not be able to smile, or their mouth or eye may have drooped arms, and the person with suspected stroke may not be able to lift their arm and keep it raised due to weakness or numbness, the person’s speech may be slurred or garbled, or they may not be able to talk at all despite appearing to be awake. The third category is Peripheral arterial disease occurs when there is a blockage in the arteries to your limbs (usually your legs). The most common symptom of peripheral arterial disease is pain in your legs when walking. This is usually in one or both of your thighs, hips, or calves. The pain can feel like a cramp, dull pain, or a sensation of heaviness in the muscles of your legs. Finally, the fourth category is Aortic disease. The Aorta is the largest blood vessel in the body. It carries blood from your heart to the rest of your body. An aortic aneurysm is the most common type of aortic disease, where the aorta’s wall becomes weakened and bulges outwards. You will usually experience pain in your chest, back, abdomen, or stomach.

Figure 2: This image shows the four main types of heart disease and what they look like from inside the human body.


Figure 3: The above graph shows the statistics on the severity of each major type of heart disease. As shown stroke seems to be the most severe at a 5, while aortic disease seems the least severe at 1. The severity scale measures the mortalities divided by the total cases and other factors like if the disease caused the patient to have a disability.

Figure 4: This graph shows the mortalities between the four major heart diseases. As you may see the most mortalities between the four major heart diseases is from coronary heart disease with 17 million mortalities every year and the least is peripheral arterial disease with only 75,000 deaths per year.
Cardiovascular Disease in the Natural and Personal Environment
Diseases and, in particular, CVDs depend on the influence of many factors. Changes in the environment can alter CVD’s risk, progression, and severity for better or worse. Scientists cannot say if Environmental changes are good for stopping the disease, but we can say that some have a bigger impact than others.
Circadian Rhythms
The first natural environment element that can affect CVDs are Circadian Rhythms. Circadian Rhythms are your body’s way of telling time between day and night. Circadian Rhythms are a direct cause of cardiovascular health and function. It is essential to go to sleep early so you do not mess up your Circadian Rhythms. If you do not, your Diurnal Cycle will be messed up, causing Myocardial Infarction which increases your risk and severity of CVD threefold.
Sunlight
The second natural environmental elements that can affect CVDs is sunlight. A well-known theory in the scientific community theorizes that less exposure to sunlight will increase the risk of CVDs. Multiple studies show that spending time outdoors inversely correlates with CVD mortality rates. Scientists theorize that Vitamin D can decrease the risk of CVDs.
Altitude
The third natural environment element that can affect CVDs is altitude. A study shows that people who live in higher altitudes have less risk for CVD because of their strong muscles near the heart and less hypertension than those near the sea.
Greenspaces
The third natural environment element that can affect CVDs are greenspaces. Greenspaces are spaces of vegetation in an area. Studies show that areas close to greenspace have lower stress levels, diabetes, stroke, and CVDs. After 100,000 trees burned in a forest fire, the citizens started to have a spike in CVDs.
Nutrition
The first personal environmental element that can affect CVDs is nutrition. One study asked nurses to change 5% of saturated fat to unsaturated fat, decreasing the risk of CVD by 42%. Mainly nutrition usually does not affect the risk of CVDs majorly, though it is still good to have a healthy diet.
Physical Activity
The second personal environmental element that can affect CVDs is physical activity. Physical activity is always a major essential for a healthy lifestyle. Physical Inactivity is a huge factor in CVDs. Studies show that if you have physical inactivity you will have 45% increase in risk of CVDs, 60% increase of stroke, 30% increase of hypertension, and T2D increase by 50%.
Smoking
The third personal environmental element that can affect CVDs is smoking. Smoking is the most negative element that can affect you by reducing 13 to 14 years of your life. Around 193 billion is lost every year in medical bills to the US, and 16% of Americans still smoke. Although smoking can cause lung cancer killing you CVDs are more common in death reports because they affect you faster.

Figure 5: This image shows that people with a cardiovascular disease who exercise more have less of a risk getting it again.
Cardiovascular Risks Associated with Gender and Aging
Aging and gender play a very important factor in the risk and severity of CVDs and other diseases. Specifically, the severity of developing cardiovascular disease is shown to increase directly and proportionally as your age also increases. CVD affects about 40% of women and men ages 40-59 and 75% of ages 60-79. Sex differences also are an important factor for CVD. The American Heart Association reports the incidence rate for CVD is 77.2% male and 78.2% female for people aged 60-79 and 89.3% for males and 91.8% for females aged 80 and above.
Pathophysiology of CVD in Aged Adults
The cause of CVD in adults is due to many factors, like oxidative stress, inflammation, apoptosis, and overall myocardial deterioration. An increase in reactive oxygen species is directly linked to persistent inflammation and progression to chronic disease. As an outcome, significant structural changes happened to the heart as they grew to cause eventual cardiac dysfunction.
Sex Differences That Arise from Hormones in Aging Adults
Differences in genders can cause discrepancies between CVD risks. Men have a stable, increasing rate of CVD risk, but women do not. Women are very prone to CVDs before and after menopause, but during the menopause period, women are not that prone to CVDs. This is due to the decline of hormones during menopause. This means that women have a very unstable risk of CVD.

Figure 6: This image shows men and women who had and haven’t had cardiovascular disease of the risk of getting it. Men in this table have a higher chance of getting cardiovascular disease compared to their respective women counterparts except when they reach age 100 the respective men and women rates are the same.
Gene Alterations and their benefit for cardiovascular disease
Cardiovascular diseases (CVDs) like arrhythmias, congenital heart disease, cardiomyopathy, high blood cholesterol, coronary artery disease, stroke, and heart failure are gene-based, meaning that we get the trait from our ancestors. Scientists in the future will use medications to change gene pairs to get rid of gene errors.
The Human Genome Project and Next-Generation Sequencing
Since genes are made of DNA, the similarities and differences in DNA are made because of the different structures and functions. Accordingly, one might reasonably expect that to investigate such similarities and differences, we must sequence and compare the DNA, anticipating distinct “genes for” not only different phenotypic traits but also many diseases caused by problems in the DNA, including cardiovascular problems. After all, the evidence for the “heritability” of a trait comes from its stronger resemblance among close relatives.
Exons, Introns, and “Alternative Splicing”
DNA coding for a protein is made of separate sections of DNA being in the same genome but separated by non-DNA strands. The coding portions of DNA are exons, and the lengths are introns. On average, there are 8.8 exons and 7.8 introns per gene. The entire DNA sequence is sent into pre-messenger RNA, but the later revising processes removes the introns, leaving the exons to determine the protein amino acid sequence. As a result, both exons and introns, as well as assorted other regulatory DNA sequences, are implicated in the RNA that guides the assembly of the protein product. Accordingly, genes should be envisioned as complex, spatially discontinuous, composite and rather not unitary objects. This is akin to the idea that a cell culture is an object. Introns were discovered by observing that the mRNA is shorter from the DNA it had been transcribed with. They are removed by splicing enzymes before mRNA, ribosomal RNA, and transfer RNA can carry out their functions.
“Junk DNA” and Regulatory DNA “Switches”
Of 3 billion DNA base pairs in the human genome, over 98 % that lie between our 20,000–25,000 genes are junk DNA with no protein coding functions, implying that DNA segments contain information to build more than just one protein through alternative RNA splicing, which details how a gene is not a continuous DNA segment. The human genome is a RNA-producing machine. The junk DNA hypothesis is being discounted as more of the non-coding DNA is found to be made into functional RNA molecules, albeit with functions not yet characterized comprehensively. The understanding of non-coding RNA transcripts is very incomplete due to enormous difficulties in genome-wide gene mining. Beyond transfer RNAs and ribosomal RNAs are classified as introns; short, long, antisense, and small interfering RNA; microRNA; and pseudogenes, and into many other functional classifications.

Figure 7: This image shows all the markers in the heart and pictures of scans on the valve.
Conclusion
Because CVDs is a common disease that affects people’s lives and causes a lot of harm to them in many ways like medical bills and quality of life decreases. The research analyzed in this research paper shows a clear connection between CVDs, gender, nutrition, physical activity, smoking, altitude, sunlight, greenspaces, Circadian Rhythms, and age. CVDs decreases life expectancy because of its severity and easy transmits. Additionally, CVDs effect on the economy increases as years go by. The implications of these findings are widespread, especially about mortality rates of CVD and prevention. For example, physicians can advise persons more susceptible to CVD to be more physically active. Another example involving CVD treatment is doctors prescribing diets without saturated fat, improving an individual’s life. In conclusion, with further research on this topic, CVDs can become a more significant task for the whole medical community, especially for those involved in cardiology.
References
Cardiovascular disease graph [Image]. (n.d.).
https://sites.google.com/a/cornell.edu/cardiovascular-disease-in-the-united-states/_/rsrc/1472855568861/home/CVD%20rates%20since%201900.png
PubMed.gov. (n.d.).
Pasipoularides A. (2015). Linking Genes to Cardiovascular Diseases: Gene Action and Gene-Environment Interactions. Journal of cardiovascular translational research, 8(9), 506–527. https://doi.org/10.1007/s12265-015-9658-9
PubMed.gov. (n.d.).
Bhatnagar A. (2017). Environmental Determinants of Cardiovascular Disease. Circulation research, 121(2), 162–180. https://doi.org/10.1161/CIRCRESAHA.117.306458
PubMed.gov. (n.d.).
Burlaton, J. P., Gourbat, J. P., & Seigneuric, A. (1991). Les facteurs de risque cardiovasculaire transmissibles [Risk factors for transmissible cardiovascular diseases]. Bulletin de la Societe de pathologie exotique (1990), 84(5 Pt 5), 677–685.
PubMed.gov. (n.d.).
Rodgers, J. L., Jones, J., Bolleddu, S. I., Vanthenapalli, S., Rodgers, L. E., Shah, K., Karia, K., & Panguluri, S. K. (2019). Cardiovascular Risks Associated with Gender and Aging. Journal of cardiovascular development and disease, 6(2), 19. https://doi.org/10.3390/jcdd6020019